Depression is one of the most common mental health conditions in the world, yet also one of the most misunderstood.
Far more than just a period of feeling low, it’s an illness that affects how people think, feel, and function in daily life. It’s both very common and very treatable, yet myths and stigma still make it hard for many people to talk about, or reach out for the treatment they need.
Knowing the basic facts of depression can make a huge difference – whether for yourself or someone you love who is struggling.
Below, we’ll share 10 important facts about depression that everyone should know, followed by answers to some of the most common questions, such as how to recognize the symptoms, how depression affects the brain, treatment options, recovery timelines, and more.
10 important facts about depression
- Depression is one of the most common mental health disorders, affecting about 5% of adults worldwide every year.
- Depression can begin at any age, but most often starts in late teens to mid-20s.
- In the U.S., more than 21 million adults (8%) and about 1 in 6 adolescents experience a major depressive episode every year.
- Depression is more than just feeling sad – it disrupts sleep, appetite, focus, energy, and daily functioning.
- Depression isn’t a weakness; it’s a medical condition that requires treatment, just like heart disease or diabetes.
- Depression isn’t caused by chemical imbalances alone; it’s a complex combination of factors that can include genetics, life stressors, medical conditions, and more.
- Only about 1 in 3 people with severe depression actually seek treatment.
- Untreated depression can last for years, and if severe, can greatly increase the risk of suicide.
- There are many types of depression, including major depressive disorder, persistent/chronic depression, seasonal affective disorder, postpartum depression, bipolar depression, and more.
- Depression is highly treatable: 70–90% of people respond well to treatment.
FAQs about depression
When you know the facts about depression – what it looks like, how it affects the brain, why it happens, and how to treat it – it becomes much easier to ask for help.
Below, we’ve answered some of the most common questions about depression in clear, simple terms. But if you think you or someone you love is suffering from depression, don’t hesitate to reach out for help.
What’s the difference between feeling sad and having depression?
Sadness is a normal emotion, but it’s usually linked to a specific event or reason, will come and go in waves, and over time will gradually ease.
Depression is much more persistent and intense. It’s a clinical mood disorder that is mostly associated with feeling sad or low, but also comes with other severe symptoms, doesn’t improve over time, and can often have no obvious cause or reason.
How do I know if I have depression?
The main symptoms of depression are a persistent sadness or low mood that lasts for at least two weeks or longer, alongside other symptoms that can start to interfere with daily life. These symptoms include changes in sleep or appetite, low energy, loss of interest in activities, difficulty concentrating, feelings of guilt or hopelessness, and in severe cases, thoughts of self-harm.
Depression is different from regular mood fluctuations because the symptoms are constant – lasting most of the day, nearly every day, for at least two weeks.
If you’re experiencing any of these feelings and think you may have depression, don’t hesitate to seek help. The only way to know for sure is to talk with a doctor or therapist, who can help identify what’s happening and guide you toward the right support.
Can children and teens develop depression?
Yes. Depression can affect children as young as 2 or 3, though it is more common in teens. Adolescents aged 12–17 are one of the main risk groups, with around 1 in 6 experiencing a major depressive episode each year.
Symptoms of depression can show differently in children and adolescents. Irritability, clinginess, refusal to go to school, trouble at school, or behavior changes are all warning signals. Other common symptoms are the same as in adults: mood changes, no longer enjoying activities they once loved, reduced energy, and changes in eating and sleeping habits. Teens with depression have a higher risk of suicide ideation compared to adults, so it’s vital to get help for any child displaying depressive symptoms as quickly as possible.
How does depression affect the brain?
Depression affects the brain both physically and cognitively – changing the way you think, feel, and process daily life.
Depression is linked to differences in brain chemistry, and if it goes on for a long time, it can also cause physical changes like brain inflammation or even shrinkage in areas that control memory and emotions.
In other words, a depressed brain often looks and functions differently than a healthy brain.
The encouraging news is that many of these effects can improve with treatment – meaning the brain has the ability to recover and heal over time.
Is depression just a chemical imbalance?
No. While brain chemistry does play a role, depression is much more complex than this. Genetics, social influences, environment, other medical conditions, and life stressors can all contribute to depression.
While scientists all agree that changes in brain chemicals are involved in depression, it’s not as simple as being “low on serotonin.” In fact, researchers still don’t know for sure whether chemical changes cause depression, or if depression itself causes those chemical changes in the brain.
What chemicals in the brain are associated with depression?
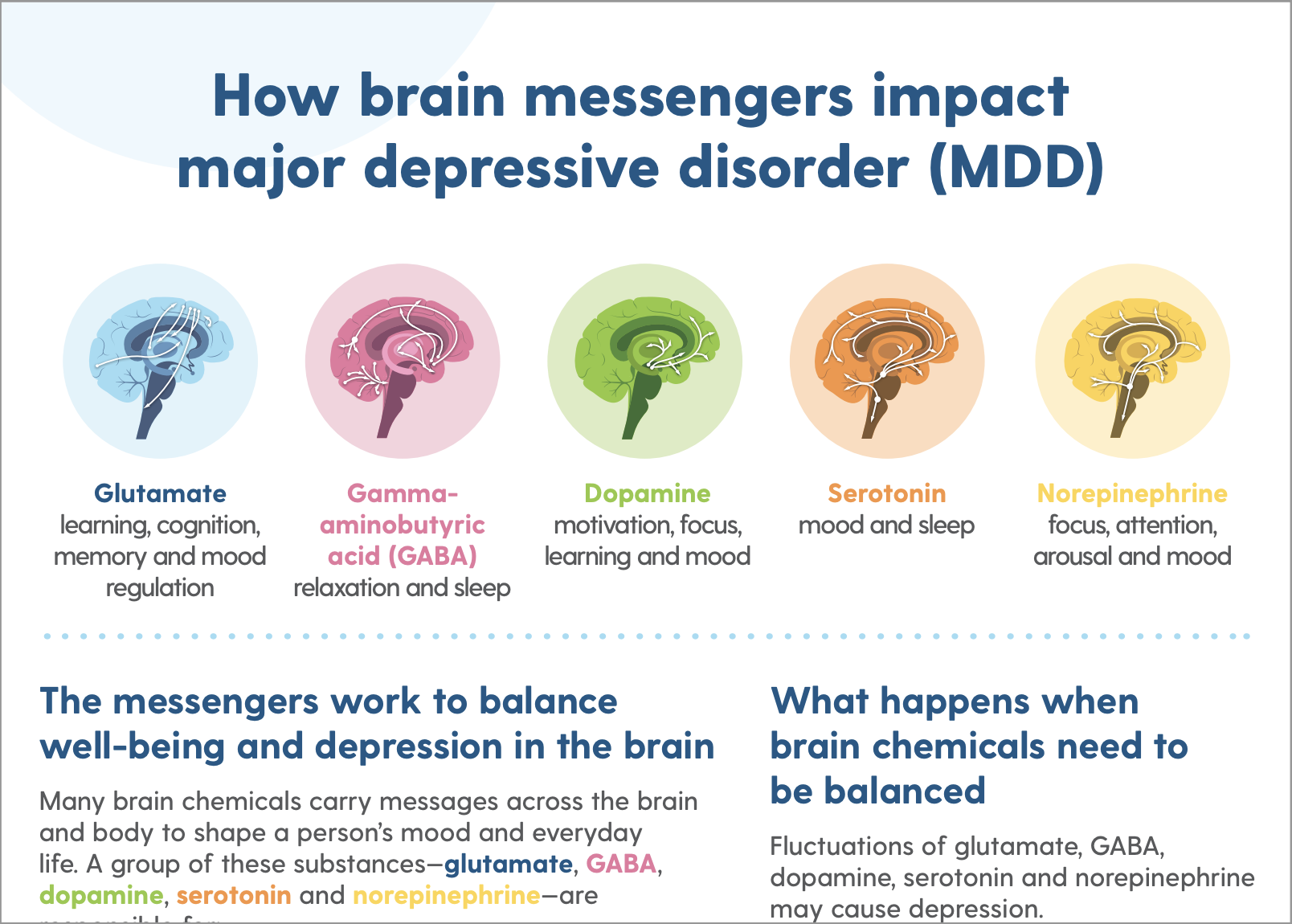
The main neurotransmitters (“brain chemicals”) associated with depression are:
- Serotonin – regulates mood, sleep, and appetite.
- Dopamine – influences motivation and pleasure.
- Norepinephrine – supports energy and focus.
- Glutamate – plays a role in memory, learning, and cognition.
- GABA – helps calm the brain and reduce anxiety.
Cortisol, the body’s main stress hormone, is also believed to play a role when levels stay too high for too long.
However, while these brain chemicals are strongly linked to depression, they don’t tell the whole story. Scientists are still uncovering exactly how depression affects the brain and why these imbalances occur, but it’s well-accepted that other factors (like genetics, environment, stress) also contribute to depression.
What is the main neurotransmitter involved in depression?
Serotonin is the most widely studied neurotransmitter in depression, which is why many antidepressants focus on it. But it isn’t the only one. Dopamine, norepinephrine, GABA, and glutamate can also play a big role.
In short, there isn’t a single “main” neurotransmitter responsible for depression. It’s the result of multiple brain systems being out of balance, usually alongside other factors like stress or genetics.
Is depression treatable?
Yes. Depression is one of the most treatable mental health conditions, and most people recover with the right care. Research shows that 70–90% of people improve significantly when they receive treatment.
For some, talk therapy alone is enough to reduce symptoms and build long-term coping skills. Medication can also provide meaningful relief, but on its own, it only addresses symptoms – not the root causes. That’s why combining medication with therapy is often the most effective approach: medication helps stabilize mood in the short term, while therapy helps untangle underlying issues and prevent relapse.
And if traditional options don’t bring enough relief, newer treatments like esketamine therapy (Spravato) are also available.
How do antidepressants work on brain chemicals?
Antidepressants work by adjusting the levels of neurotransmitters – the brain’s chemical messengers – that affect mood, energy, and motivation.
Different types of antidepressants target different neurotransmitters:
- SSRIs (like Prozac or Zoloft) regulate serotonin.
- SNRIs (like Cymbalta or Effexor) regulate serotonin and norepinephrine.
- Other types can affect dopamine and related pathways.
By restoring balance in these systems, antidepressants help ease symptoms like sadness, fatigue, and poor concentration. However, it’s important to understand that antidepressants only treat the symptoms; they don’t resolve any of the other underlying causes of depression. That’s why they’re most effective when combined with talk therapy.
How long does depression usually last if treated?
With treatment, many people notice improvement within 4–8 weeks, though full recovery usually takes several months.
Antidepressants generally take at least 4 weeks to bring relief. Talk therapy (whether on its own or combined with medication) also typically requires at least one month before significant results are seen, with steady gains from there.
Ongoing therapy is especially valuable for preventing relapse, since medication alone treats symptoms but not underlying causes. Therapy provides coping tools and addresses patterns that drive depression, making recovery more sustainable.
What if I have a “crippling depression” that doesn’t improve?
If your depression isn’t improving with standard treatments like therapy and medication, you may have treatment-resistant depression (TRD). This doesn’t mean recovery isn’t possible – it just means your brain may need a different approach.
Thankfully, a new medication has recently been developed and FDA-approved specifically for treatment-resistant depression: esketamine therapy (Spravato).
Delivered as a nasal spray, it works on a different brain pathway than traditional antidepressants and can bring relief much more quickly – sometimes within 24 hours. Many people who didn’t respond to other treatments have found it life-changing.
At REACH, our psychiatrists and therapists work together to create personalized treatment plans. Even if your depression feels crippling, know that effective treatment options exist, and you don’t have to face it alone.
Find relief from depression at REACH Behavioral Health Ohio
Depression is one of the most treatable mental health conditions, yet many people delay getting help. That’s why it’s so important to know the facts about depression: it’s common, it’s a medical condition – not a weakness – and with the right treatment, most people recover.
Left untreated, depression can grow more severe and affect every part of life: work, relationships, health, and overall well-being. But with proper care, many people start feeling relief within just a few weeks and continue improving over time.
At REACH Behavioral Health, we make treatment easier by offering both therapy and psychiatry under one roof. Whether it’s talk therapy, antidepressants, or Spravato ketamine therapy for treatment-resistant depression, our team will help you find the approach that fits your needs best.You don’t have to face depression alone. Reach out to us today, and take the first step toward steadier days and a brighter future.

