Trauma can come in many different forms and mean many different things, but almost everyone will experience some kind of trauma in their lifetime.
Whether it stems from a single event or prolonged exposure to distressing situations, trauma can deeply affect mental, emotional, and physical well-being, and if left untreated, it can leave a lasting impact on a person’s life.
Trauma therapy is the primary means of helping people heal from traumatic experiences, but the great news is that there is now such a significant awareness of trauma and its impacts that the six core principles of trauma-informed care (TIC) are becoming increasingly adopted throughout all kinds of healthcare, educational, and other organizational settings – it’s no longer limited just to the realm of therapy and mental health treatments.
For those seeking help, it’s useful to understand the distinction between trauma-informed care and trauma therapy. So in this article, we’ll explore the six core principles of trauma-informed care (TIC), their role in trauma therapy, and how we at REACH Behavioral Health Ohio integrate these principles into our services to support your healing and recovery.
What is trauma and how does it affect people?
Trauma is defined as an emotional and psychological response to a deeply distressing or disturbing event. However, the “types” of events that can cause trauma are far-ranging, just as the impacts of trauma can manifest in many different ways.
Many people associate trauma with significant specific events, such as abuse, accidents, the loss of a loved one, or experiencing things such as extreme violence or natural disasters. But trauma can also result from ongoing exposure to adverse conditions, such as childhood neglect, domestic violence, or prolonged stress, and in some cases it can even stem from experiences that may be perceived as “normal” to others in a better condition to cope.
The effects of trauma are just as diverse, manifesting in physical, emotional, or behavioral symptoms that can range as broadly as from flashbacks and nightmares to difficulty concentrating, emotional numbness, anxiety and depression, isolation and avoidance, fatigue and headaches, and much more – all of which can significantly disrupt daily life and overall well-being.
For some, the effects of trauma may be short-term, while others might struggle with trauma symptoms for years. But most important is to recognize that everyone processes trauma differently.
Understanding trauma-informed care vs. trauma therapy
If you or a loved one is suffering from trauma and seeking help, you may have come across the terms trauma-informed care and trauma therapy, and be wondering exactly how they differ.
While the two terms have many similarities and overlaps, they are fundamentally different things:
Trauma therapy
Trauma therapy, or trauma-focused therapy, is a type of psychotherapy designed to help individuals process and heal from specific traumas they have experienced.
As with other types of talk therapy, trauma-focused therapy encompasses various therapeutic approaches depending on the individual’s unique needs and situation. These include Cognitive Behavioral Therapy (CBT), Dialectical Behavioral Therapy (DBT), Prolonged Exposure (PE), as well as body-based therapies such as Eye Movement Desensitization and Reprocessing (EMDR). Both individual therapy and group therapy can be very helpful for people working through the impacts of trauma.
Trauma-informed care (TIC)
Trauma-informed care, on the other hand, is not about treating any one trauma but is instead a framework, or an approach, that recognizes the impact trauma can have on a person.
It’s an approach that can be (and is, increasingly) used in various settings – including healthcare, social services, education, and other organizations – that emphasizes the importance of recognizing and responding to the impact of trauma.
Essentially, it’s about shifting from a mindset of “What’s wrong with you?” to “What happened to you?” and recognizing that it’s necessary to have a complete picture of a person’s life situation – both past and present – in order to provide effective care.
TIC is therefore not a specific treatment, but a more generalized way of delivering care that integrates knowledge about trauma into policies, practices, and procedures, with the aim of creating environments that are safe, supportive, and empowering for everyone.
In short – trauma-informed care is about providing supportive environments that acknowledge the impact of trauma, whereas trauma therapy actively works on resolving and processing a specific trauma. But the two concepts are very much interlinked.
The 6 core principles of trauma-informed care
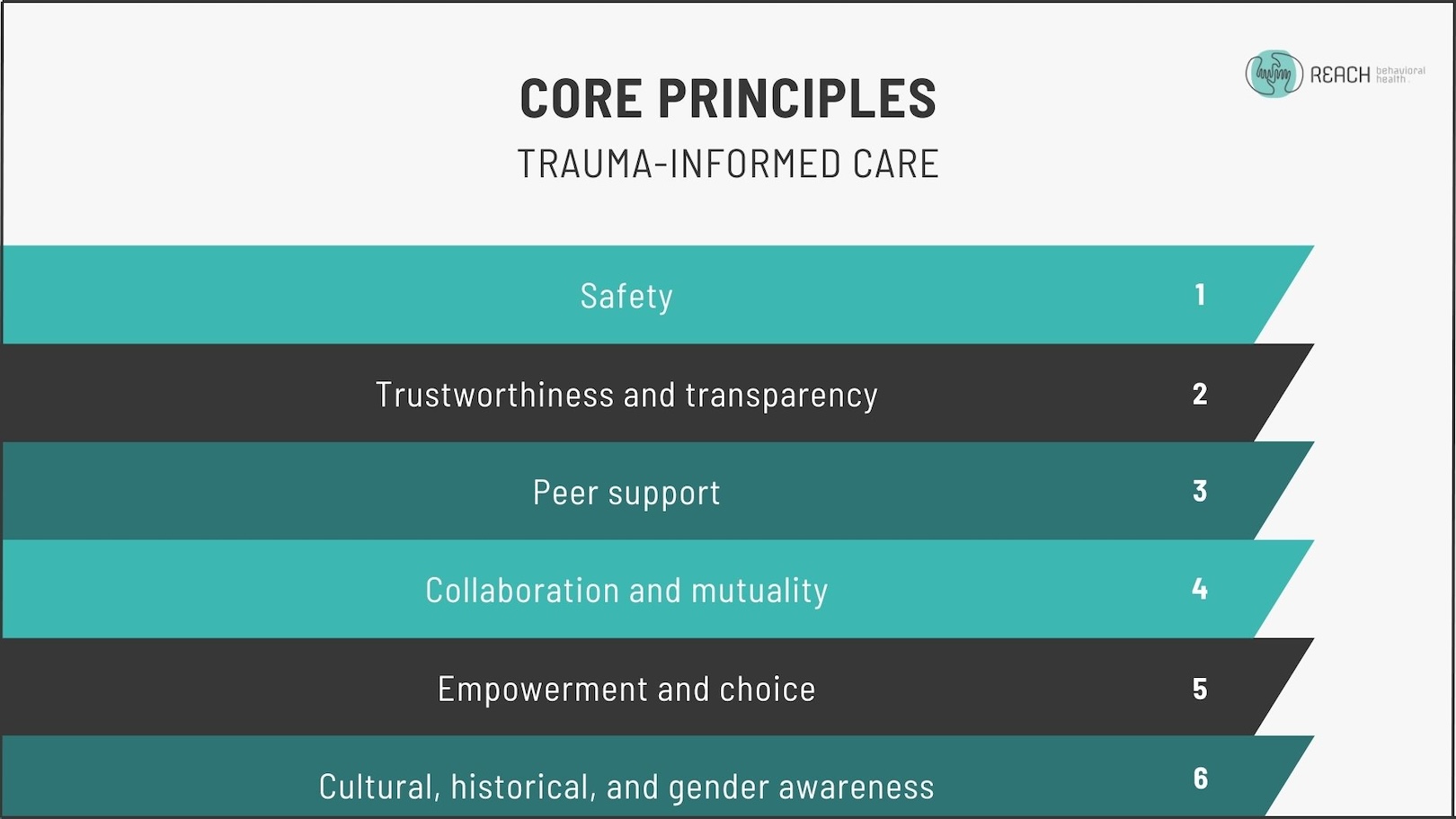
There are six guiding principles of trauma-informed care that underlie its approach.
These principles are vital aspects of effective trauma therapy, and as such should always be applied to trauma-related therapuetic and mental health services.
But the concept behind TIC is that they can also be applied generally throughout other workplace, educational, or organizational settings to help create environments that promote healing and avoid re-traumatization.
The six core principles of TIC are:
- Safety: Ensuring physical and emotional safety for everyone involved.
- Trustworthiness and transparency: Building trust through clear communication and consistency.
- Peer support: Encouraging shared experiences to build community and support.
- Collaboration and mutuality: Emphasizing partnership and minimizing power dynamics by sharing decision-making and responsibility.
- Empowerment and choice: Prioritizing individual strengths and offering choices in decision-making processes to encourage active participation in achieving one’s own goals.
- Cultural, historical, and gender awareness: Acknowledging and addressing the cultural and societal contexts that influence a person’s experience of trauma.
How trauma-informed care supports trauma therapy
When looking specifically at treating trauma, it’s clear to see how TIC lays the groundwork for effective trauma therapy.
Here are examples of how trauma-informed care supports and complements effective trauma therapy:
- Creating a safe space: Establishing safety and trust is crucial for effective therapy. It allows clients to explore and process traumatic memories without fear of re-traumatization. This foundation of safety helps reduce anxiety and encourages deeper therapeutic work.
- Building trust and transparency: Clear communication, honesty, reliability, and consistent boundaries help build a trusting relationship, which is essential for clients to feel comfortable and engaged in therapy.
- Empowerment and choice: Trauma survivors often feel powerless, so giving them a voice in their treatment – such as choosing which therapeutic approach to use or setting personal goals – helps them feel more engaged and invested in their recovery, and restores a sense of control.
- Collaboration and mutuality: Emphasizing partnership in therapy, where clients and therapists co-create treatment goals and strategies, helps level power dynamics and makes clients feel like equal partners in their healing journey.
- Cultural sensitivity: People from marginalized communities or backgrounds often experience discrimination that can have a significant impact on their trauma experience or response. Therapists must be aware, educated, and understanding of these cultural factors to ensure the therapy is relevant, respectful, and effective.
- Peer support: Utilizing peer support, such as via day treatment programs or group therapy, can help clients feel less isolated. Knowing others have experienced similar struggles fosters a sense of belonging and validation, which is essential for healing.
- Trauma awareness in all interactions: From the initial phone call to each therapy session, every interaction should reflect an understanding of trauma’s impact. This ensures clients feel safe and respected at all stages of their care.
Getting started with trauma therapy at REACH
One of the most important things to remember about trauma is that it is extremely common – it’s estimated that over 70% of American adults have experienced some kind of traumatic event in their lifetime. Yet it’s often left unaddressed.
If you’ve experienced a traumatic event that you’re struggling to ovecome, it’s important to know that you’re not alone and that help is available.
At REACH Behavioral Health, our experienced therapists will work with you to understand your needs, develop a personalized treatment plan, and guide you through your healing journey.
With the principles of trauma-informed care underlying all our therapeutic services, we’re ready to provide the safe space and expert care that you need to work through the impacts of your trauma, heal, and move forward with your life.

